Benign Hematological Disorders ( Adult & Paediatric)
Benign hematological disorders refer to non-cancerous conditions that affect the blood, bone marrow, or the lymphatic system in both adults and children. These disorders can involve abnormalities in red blood cells, white blood cells, platelets, or the coagulation system. Although not malignant, they often require precise diagnosis and effective management due to their impact on a patient’s health and quality of life.
Common Benign Hematological Disorders
1. Anemias:
- Iron Deficiency Anemia: Caused by insufficient iron, leading to reduced red blood cell production.
- Megaloblastic Anemia: Due to deficiencies in vitamin B12 or folate.
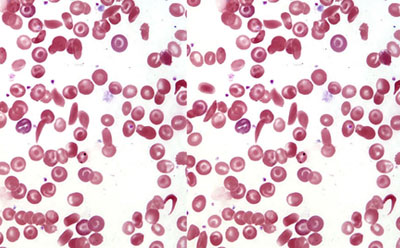
- Hemolytic Anemia: Premature destruction of red blood cells (e.g., autoimmune hemolytic anemia, hereditary spherocytosis).
- Aplastic Anemia: Failure of bone marrow to produce sufficient blood cells.
2. Bleeding Disorders:
- Hemophilia A and B: Genetic conditions resulting in deficient clotting factors VIII or IX.
- Von Willebrand Disease: Deficiency or dysfunction of von Willebrand factor affecting platelet adhesion.
- Thrombocytopenia: Low platelet count due to immune or non-immune causes (e.g., ITP, drug-induced).
3. Clotting Disorders:
- Thrombophilia: Increased tendency to form blood clots (e.g., Factor V Leiden mutation, Protein C or S deficiency).
- Disseminated Intravascular Coagulation (DIC): A complex disorder causing simultaneous clotting and bleeding.
4. White Blood Cell Disorders:
- Neutropenia: Low levels of neutrophils, increasing infection risk.
- Leukocytosis: Abnormally high white blood cell counts due to reactive or hereditary conditions.
5. Hemoglobinopathies:
- Thalassemias: Genetic disorders leading to abnormal hemoglobin production (e.g., Alpha and Beta Thalassemia).
- Sickle Cell Disease: Abnormal hemoglobin S causing red blood cells to assume a sickle shape.
6. Bone Marrow Disorders:
- Myeloproliferative Disorders: Overproduction of blood cells, such as in essential thrombocythemia or polycythemia vera.
- Myelodysplastic Syndromes (non-malignant forms): Ineffective blood cell production.
Management Strategies
Diagnosis:
- Comprehensive blood tests (CBC, peripheral smear, reticulocyte count).
- Bone marrow aspiration and biopsy when required.
- Specialized tests, including genetic studies, coagulation profiles, and hemoglobin electrophoresis.
Treatment Options:
- Nutritional Therapy: Iron, vitamin B12, or folate supplementation for nutritional anemias.
- Blood Transfusions: For severe anemia or symptomatic hemoglobinopathies.
- Medications:
Immunosuppressants for autoimmune disorders.
Growth factors like erythropoietin or G-CSF for bone marrow stimulation. - Replacement Therapy: Clotting factors for hemophilia or von Willebrand factor concentrates.
- Bone Marrow Transplantation (BMT): For severe aplastic anemia or genetic disorders.
- Anticoagulants or Antiplatelet Drugs: For clotting disorders.
Supportive Care:
- Management of infections in immunocompromised patients.
- Pain relief and hydration for sickle cell crises.
- Regular monitoring to prevent complications.
Goals of Management
- Control symptoms and improve quality of life.
- Address underlying causes where possible.
- Prevent complications such as organ damage, infections, or clotting events.
- Educate patients and families about the condition and its long-term care.
